Symptoms and Causes of Tinea Unguium
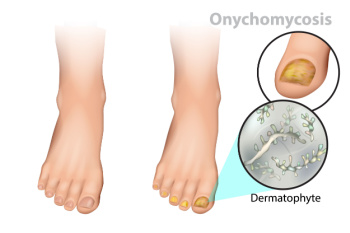
Tinea unguium, also known as onychomycosis, is a fungal infection that affects the nails, particularly the toenails. This condition causes changes in the appearance of the nails, which may become thickened, discolored, and brittle. Infected nails can also separate from the nail bed, causing discomfort and potential pain. The primary cause of tinea unguium is the overgrowth of fungi, particularly dermatophytes, which thrive in warm and moist environments. Risk factors include wearing tight footwear, having a history of athlete's foot, and compromised immune systems. Poor hygiene can also contribute to the development of this infection. Recognizing the symptoms early is essential for effective treatment, as untreated cases can lead to more severe complications. If you have toenail fungus symptoms, it is suggested that you consult with a podiatrist who can offer you prescribed medication for effective treatment.
For more information about treatment, contact Gary Saphire, DPM of Parkway Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact our office located in Brooklyn, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Toenail Fungus
Toenail fungus is a frustrating problem that affects many people. It can be persistent and hard to get rid of. As many different types of fungi are present throughout the environment, it is very easy to contract toenail fungus.
The feet are especially susceptible to toenail fungus because shoes and socks create the ideal dark and moist environment that fungal infections thrive in. While fungal infections of the nail plate are quite common, if left untreated they can spread beyond the toenail and into the skin and other parts of the body.
Signs of toenail fungus include a thickened nail that has become yellow or brown in color, a foul smell, and debris beneath the nail. The toe may become painful due to the pressure of a thicker nail or the buildup of debris.
Treatment for toenail fungus is most effective during the early stages of an infection. If there is an accumulation of debris beneath the nail plate, an ingrown nail or a more serious infection can occur. While each treatment varies between patients, your podiatrist may prescribe you oral medications, topical liquids and creams, or laser therapy. To determine the best treatment process for you, be sure to visit your podiatrist at the first signs of toenail fungus.
Peripheral Artery Disease and the Feet

Peripheral arterial disease, or PAD, occurs when blood vessels in the legs and feet become narrowed or blocked, reducing blood flow. The most common cause of PAD is atherosclerosis, where fatty deposits build up in the arteries, restricting circulation. This lack of blood flow affects the feet by causing pain, cramping, or fatigue, especially during walking or physical activity, a condition known as claudication. In severe cases, PAD can lead to non-healing sores or ulcers on the feet and toes, and in extreme cases, gangrene. Symptoms of PAD in the feet include coldness, a bluish tint, or slow-healing wounds. Since diabetes and smoking increase the risk of PAD, managing these conditions is essential. If you have peripheral artery disease it is suggested that you visit a podiatrist who can help monitor foot health, and provide care to prevent further damage.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Gary Saphire, DPM from Parkway Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Painful Corns

Corns are a common skin condition, with distinct characteristics and causes. Corns are thickened patches of skin that develop due to friction or pressure, often on the toes or soles. They are usually smaller than warts and have a hard center surrounded by inflamed skin. Symptoms of problematic corns include localized pain and tenderness. Wearing shoes with plenty of room for the toes is the best way to prevent corns. If your toes cannot wiggle and move around, the shoes are likely too tight. Persistent corns that cause significant discomfort may require medical intervention. A podiatrist may recommend cryotherapy, laser treatment, or surgical removal. If you have corns that do not improve, it is suggested you schedule an appointment with a podiatrist for a thorough evaluation and effective treatment options.
Corns can make walking very painful and should be treated immediately. If you have questions regarding your feet and ankles, contact Gary Saphire, DPM of Parkway Podiatry. Our doctor will treat your foot and ankle needs.
Corns: What Are They? And How Do You Get Rid of Them?
Corns are thickened areas on the skin that can become painful. They are caused by excessive pressure and friction on the skin. Corns press into the deeper layers of the skin and are usually round in shape.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as:
- Wearing properly fitting shoes that have been measured by a professional
- Wearing shoes that are not sharply pointed or have high heels
- Wearing only shoes that offer support
Treating Corns
Although most corns slowly disappear when the friction or pressure stops, this isn’t always the case. Consult with your podiatrist to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our office located in Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Corns and Calluses
A corn is a lesion that forms in the skin of the foot, and it is typically circular in shape, small in size, and thick and rough in texture. A corn generally occurs as a result of repeated pressure on the skin; one example of this is the rubbing of a shoe against the skin. Corns differ from calluses in that their central cores are harder in texture.
A corn is a relatively common condition with a wide variety of treatment options. If a corn becomes overly uncomfortable or painful, consult with your podiatrist; he can determine the best method of treatment that is appropriate for you. Corns may return if the underlying cause of its development is not treated or removed. Avoid removing corns at home, as improper removal may cause infection.
A callus, similar to a corn, is an area of skin that has become thickened due to repeated pressure and rubbing. The rubbing causes the skin to create a layer of protective skin, which is the formed callus. Calluses can differ in size between people, and they can also become painful.
Multiple treatments are available for calluses. At-home treatment and removal should be avoided, as this can potentially lead to infection. Your podiatrist can best determine the cause of your calluses and suggest the treatment most appropriate for you.
Preventing Same Level Falls in the Workplace

Same level falls occur when individuals trip, slip, or stumble on surfaces at the same height they are standing on, often leading to injuries that can affect productivity and morale. To prevent these incidents in the workplace, it is vital to implement several strategies. First, using appropriate flooring can significantly reduce the risk. Non-slip surfaces are ideal in high-traffic areas. Regularly removing obstacles such as clutter, cords, and equipment can create a safer environment. Promptly cleaning up spills and ensuring that wet floors are marked with clear signage is essential for alerting employees to potential hazards. Additionally, wearing protective gear, such as slip-resistant shoes, can further enhance safety. Falling can seriously impact the feet, which may cause a loss of work and wages. If you have had a foot injury from falling, it is suggested that you consult a podiatrist who can treat various foot injuries, and guide you on appropriate fall prevention methods in the work environment.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Gary Saphire, DPM from Parkway Podiatry. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
Facts About Dislocated Toes

A dislocated toe occurs when the bones in the toe become misaligned, often leading to significant discomfort and mobility issues. Common symptoms include intense pain at the site of the injury, noticeable swelling, and bruising. The affected toe may appear deformed or out of place, and there may be difficulty moving it or walking without pain. Several factors contribute to dislocated toes, with sports injuries being a leading cause. Activities involving running, jumping, or sudden changes in direction can put excessive stress on the toe joints. Also, accidents such as stubbing the toe or dropping a heavy object on it can lead to dislocation. If you have sustained an injury that may have dislocated your toe, it is suggested that you promptly contact a podiatrist who can provide an accurate diagnosis and treatment.
Toe pain can disrupt your daily activities. If you have any concerns, contact Gary Saphire, DPM of Parkway Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please feel free to contact our office located in Brooklyn, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.